At Henry Community Health, we look for solutions that enable us to be agile in our adoption and lower our infrastructure footprint. symplr Workforce, specifically the self-scheduling mobile functionality, has been a game changer for our organization. As a long-standing customer of symplr, the experience migrating to symplr Workforce has elevated us from a vendor/customer relationship to a true partnership.
Healthcare Workforce Management | symplr Workforce
Workforce management built for healthcare's complexities
Healthcare is complicated, and workforce management is one of the most complicated systems there is. Tracking time and all the pieces involved requires software that can navigate the unique demands of healthcare. At symplr, we are proud to provide healthcare-specific solutions to manage the complexities of timekeeping and scheduling, freeing up nurses to have more time for patient care.
Karlene Kerfoot, PhD, RN, FAAN
Chief Nursing Officer, symplr


Invested in too many disparate systems to manage your healthcare workforce?
To combat workforce shortages, increased labor costs, and other challenges, healthcare leaders are investing in technology.
What they fail to realize…
The use of disconnected systems may exacerbate workforce problems at your organization. According to the symplr Compass Survey, health system leaders are frustrated by working with too many siloed systems.
There's a better way.
Integrated, healthcare-specific workforce management technology helps reduce administrative burden and gives clinicians time back for patient care.
A collaborative and efficient workforce management approach can help your organization retain staff, contain costs, and improve patient care.
Workforce management built exclusively for healthcare
symplr has decades of experience delivering customer outcomes for hospitals and health systems.
Optimize staff, contain costs
Engage and retain staff
Remain compliant
Powerful, integrated workforce management
Give managers and staff robust, mobile capabilities
Access to real-time data to contain costs and remain compliant
Gain clear, enterprise-wide visibility
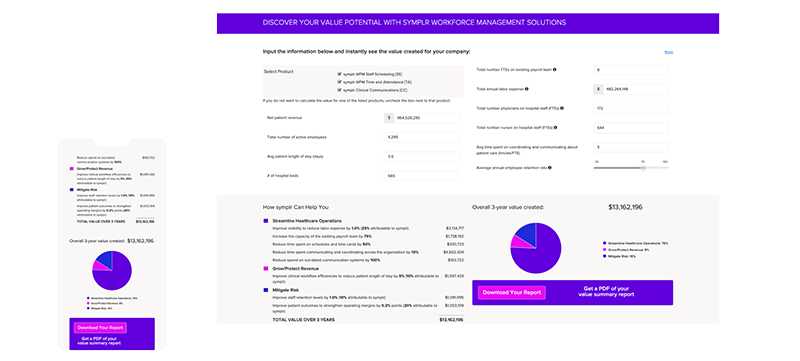
Calculate potential gains with the use of symplr Workforce Management
symplr Workforce customers have reported:
- 50% reduction in time spent managing timecards and schedules
- 75% increase in the capacity of current payroll team
Enter a few data points into our calculator to get a custom report estimating the potential cost savings of using symplr Workforce Management solutions.
Ranked #1 in Ease of Administration
G2 crowd category winner for Medical Staff Scheduling, Healthcare HR, and Enterprise Healthcare HR













G2 names symplr a High Performer
Enterprise Spring 2024
G2 names symplr a Leader
Spring 2024
G2 names symplr a Momentum Leader
Spring 2024
G2 names symplr a High Performer
Enterprise Winter 2024
G2 names symplr a Leader
Winter 2024
G2 names symplr a High Performer
Enterprise Fall 2023
G2 names symplr a High Performer
Fall 2023
G2 names symplr a Momentum Leader
Fall 2024
G2 names symplr a High Performer
Enterprise Summer 2023
G2 names symplr a High Performer
Summer 2023
G2 names symplr a High Performer
Enterprise Spring 2023
G2 names symplr a High Performer
Winter 2023
G2 names symplr a High Performer
Enterprise Winter 2023
What our symplr Workforce customers are saying
MIKE SPENCER
CIO, Henry Community HealthREGINA M. BERGH
Financial Controller, Bryan HealthEVELYN OLENICK
SVP and Chief Nursing Officer, Phoebe Putney Health SystemKATHLEEN RANGEL
IT Shared Business Services Lead, Genesis Health SystemADAN FRIEDLI
System Administrator, Mary Free Bed Rehabilitation HospitalLORI FROST
MercyCaresymplr healthcare workforce management